The Effects of Crystal Meth Use
Methamphetamine is a highly addictive stimulant that can have long-lasting effects on your body. This is a man-made substance that, with the advent of other more efficacious prescription stimulants, now has limited therapeutic use and is only very rarely indicated for intractable ADHD and severe obesity.
The illicut drug crystal meth is methamphetamine in the form of a rock-like crystal that is usually a semi-transparent white or blue color. This substance is always illegal and has no other purpose than for abuse.
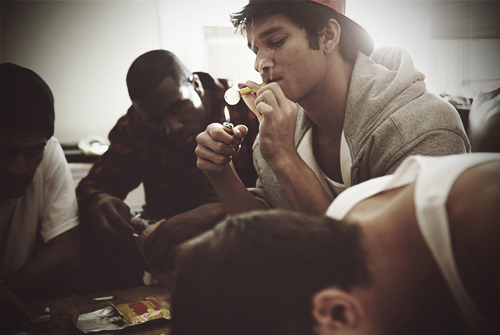
Crystal meth is mostly heated and then smoked in a glass pipe. Less frequently, the drug is crushed up to be snorted or injected. Smoking it speeds the delivery of the substance into the bloodstream, which further promotes the addictive nature of the substance.
Side Effects
Other side effects of crystal meth include:
- Loss of appetite.
- Significant weight loss.
- Change in sleeping patterns.
- Severe mood swings.
- Unpredictable behavior.
- Tremors or convulsions.
- Hyperthermia.
- Elevated blood pressure.
- Rapid heart rate.
- Irregular heart rhythm.
Consistent use of crystal meth can result in severe anxiety, paranoid and insomnia. Additionally, thoughts of suicide—or even homicide—have been noted in some meth abusers.
Some people take crystal meth to experience a specific set of stimulant side effects. This includes the decrease in appetite, increased energy levels, and increased metabolism that some users attempt to take advantage of to achieve weight-loss. The drug also tends to increase libido, leading to abuse of the drug for that purpose alone.
It’s safe to say that none of the perceived short-term benefits of a dangerous drug are worth the risk of developing a deadly dependency that comes with them.
Long-Term Effects
Taken over a long period of time, crystal meth can cause severe physical and psychological issues as the short-term effects grow in intensity and complexity. Signs of long-term cystal meth abuseinclude:
- More persistent psychotic symptoms–including delusions, paranoia, and hallucinations.
- Increased mental health issues like depression, anxiety and social isolation.
- Confusion and odd behavior.
- Feeling of bugs crawling on the skin.
- Body sores from users picking at their skin.
- Breathing problems associated with smoke inhalation.
- Irreversible damage to blood vessels throughout the body, including the heart and brain.
- Stroke.
- Coma.
Severe crystal meth abuse can also cause outward signs of aging in users. Since the drug destroys tissues and blood vessels and hampers the body’s ability to heal, users often develop acne, and the skin takes on a dull look and loses its elasticity. The teeth can begin to decay and crack, resulting in a condition known as “meth mouth.”One of the most serious long-term side outcomes of crystal meth, however, is sudden death from cardiac arrest or stroke.
Crystal Meth Dependency
Crystal meth signals the brain to fire off an increased amount of dopamine, a chemical that causes a feeling of reward or pleasure.
The increased activity of dopamine is what scientists believe plays a large role in the development of addiction to certain drugs. It is thought that the positive feeling from dopamine is so strong—and intensely rewarding—that it reinforces the behavior that initiated its release.
As users become more tolerant of crystal meth, they will need more of the substance to achieve the desired high and will take ever-increasing amounts, placing themselves at risk for overdose and furthering fueling the body’s dependency on the drug.
Over time – after a period of persistent stimulant intoxication – dopamine receptor activity is severely impaired, which can cause perceptions of decreased happiness and pleasureand even lead to permanent cognitive impairments.